Imagine if everyday tasks suddenly became a struggle—not just walking, but going to school or playing sport. That’s the reality for children living with Juvenile Dermatomyositis (JDM), a rare autoimmune disease that affects just two to three new children per million each year. The condition causes the body to attack its own cells, leading to muscle pain, skin rashes and severe physical weakness.
JDM affects an estimated one in 20,000 children, with girls around twice as likely to be diagnosed as boys. Yet media coverage remains limited, contributing to low public awareness of the condition.
“If you’ve never seen a child with JDM before, it’s a pattern that is very difficult to put together,” said Dr Lucy Wedderburn, professor of paediatric rheumatology at Great Ormond Street Hospital and University College London. “The child is a bit more tired than usual, perhaps wants to sit out of PE before the end of the hour, and starts to have difficulty getting out of the bath or up the stairs.”
The disease causes intense fatigue, muscle pain, unexplained fevers and a distinctive rash that is often misdiagnosed as eczema or psoriasis. Swelling can also occur around the eyes, muscles, tissues and joints.
Diagnosing JDM is a lengthy and complex process, often involving blood tests, MRI scans and X-rays, and in some cases, a muscle biopsy. Treatment is equally challenging. Dr Penny Davis, a consultant in paediatric rheumatology at Birmingham Children’s Hospital, explains:
Although treatment is incredibly intense and upsetting for the child and their family, it has proved to be effective. “Most children with JDM live with their condition well, go back to school, join sports, and theirs lots of personal stories like that so it’s important to find ways to hold onto that hope,” said Dr Wedderburn.
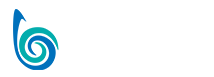
Seventeen-year-old Amelia Sharpe is an example:
Amelia shares an incredibly powerful story about how low things got for her, but one of the things that made it easier was having such a strong support system around her.
“It’s something that you might of heard of once at medical school, but possibly not,” said Dr Davis. “Even in a big centre like Birmingham or Great Ormond street the numbers of patients we have with JDM are very low so a young person is not going to have come across another patient with the condition and it’s very isolating.”
This means connecting with other families going through the same challenges is really important. There are many patient support groups and charities who bring people together, including Southampton based charity, Myositis UK. Set up by Irene and Les Oakley in 1985, after their daughter was diagnosed with Juvenile Dermatomyositis, they provide information packs, raise funds for research, and host an annual conference to help connect those going through similar experiences.

Photo courtesy: Irene Oakley
“When we started off, all we had was a typewriter on the kitchen table,” said Irene Oakley. The charity she helped build, Myositis UK, now has around 600 members and has funded £120,000 worth of research in the past 18 months.
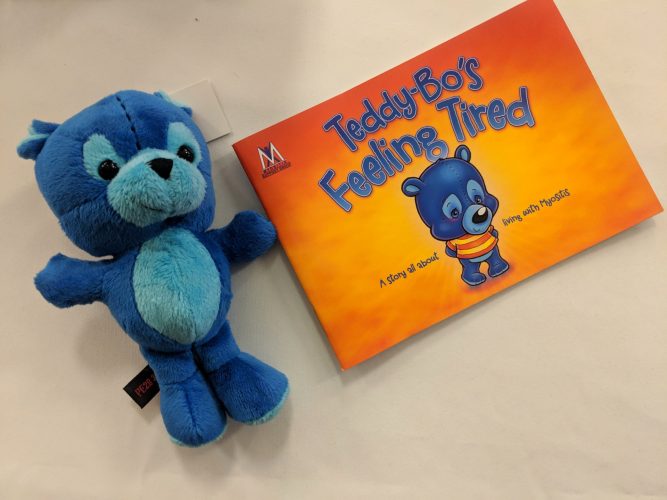
The charity has developed resources to support families affected by JDM, including the Teddy Bo book. “It’s a resource not only for the child with the illness, but also for siblings — to help them understand what’s happening,” said Irene.
“One of the main things we funded were two workshops at Great Ormond Street in muscle biopsy examinations,” Irene continued. Specialists from Brazil, the USA, Europe and across the UK attended. The workshops laid the groundwork for future research, helping define key features in biopsies used to diagnose myositis. Fifteen years later this work is being published as a gold standard worldwide for using muscle biopsies to diagnose myositis.
Advances in myositis research has meant professionals can now identify what type of JDM patients have, based on the type of antibodies that present. This work, funded by Myositis UK, has significantly improved the treatment process, allowing treatment to be personalised. Dr Wedderburn explains:
That’s one example of the improvements in JDM diagnosis, and there are advancements in the treatment process as well. Dr Davis explains:
Although these developments mark significant progress in JDM care, much work remains. “Because of its rarity, many GPs and even hospital doctors will never see a case of JDM,” said Irene.
Myositis UK is working to change that by contacting medical bodies to have myositis included in basic training. Irene’s biggest hope is that “every doctor has some knowledge of JDM and every doctor who sees it will refer that child to a specialist centre”.
Irene discussed other improvements to JDM treatment that need to be the focus moving forward:
There is hope for the future of JDM care. For anyone living with Juvenile Dermatomyositis — whether a child, friend or family member — this story stands as a reminder of resilience. Like Amelia, many do go on to overcome the challenges of JDM.
See Myositis UK
Cover image: Amelia Sharpe, at Birmingham Childrens Hospital in June 2019. Photo courtesy: Susie Sharpe