*TRIGGER WARNING: THERE ARE REFERENCES OF A SEXUAL NATURE AND SUICIDE WITHIN THIS ARTICLE*
Contraception, everyone has a story about it… the good, the bad, the accidentally pregnant. But after talking to large numbers of women over the years, friends and family included, it’s forced me to ask myself, why is there not more education about contraception and women’s health?
With millions of women in the UK alone on various forms of contraception and the average age girls first start using contraceptives being 15, it’s surprising that many people, all genders included, do not know of the many health complications and benefits that various methods of contraception can provide.
My own experience fits into this too, and I personally have gone through some awful side effects, life changes and procedures all in the name of trying to enjoy sex and avoid pregnancy. This includes two types of ‘the pill’, a mini pill, the patch, and three copper IUD’s. As well as passing out on a London underground carriage, suicidal thoughts, a million days of awful period type cramps (or so it feels), horrific vaginal injections, and gas and air on more than one occasion, all in 10 years alone!
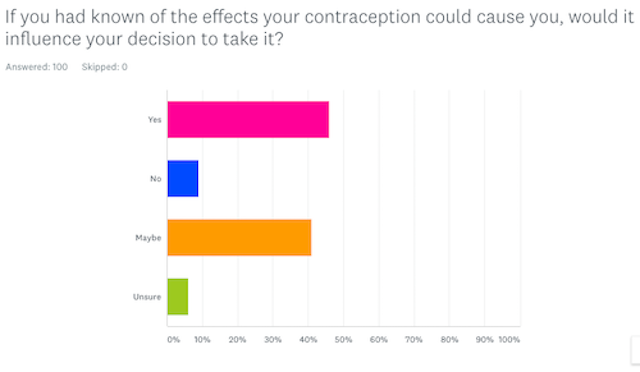
Today it is estimated (at time of publication, from a 2008 study by the Office for National Statistics) that 3.5 million women are taking the contraceptive pill and 75 percent of women aged 16-49 are on some form of hormonal contraceptive. Plus, when conducting a survey of my own of 100 participants (with 96 of participants identifying as women) I asked: “if you had known of the effects your contraception could cause you, would it influence your decision to take it?” A staggering 46 percent answered yes and 47 percent saying maybe, or they were unsure. This could also suggest why 59% percent reported they had had a bad experience in some way with at least one form of contraception or multiple forms!
In relation to contraception as a medicine then it is also problematic to women’s health, and not only because many women take it to prevent pregnancy. According to women’s health practitioner Maisie Hill, “56 per cent of contraceptive pill users are using it for non-contraceptive reasons, with 31 per cent of this to lower menstrual pain and 9 per cent never of having sex”.
On a positive note, the discussion surrounding contraception has become wider and more publicly acknowledged, especially amongst women as the years have gone by. It’s now frequently discussed in women’s magazines and blogs, with 57,464 posts featured on Instagram with the hashtag #Contraception (as of the 20th of August 2020), several podcasts across platforms such as iTunes and Spotify, and websites such as #MYCONTRACEPTION becoming available and widely used. Not only this, but male contraceptives are becoming a more popular and realistic conversation too, with articles featuring in common women’s magazines and websites including GLAMOUR online in their August 2018 edition and Cosmopolitan in their June 2020 print magazine.
However, many women are still unsure of what methods they can use, or the benefits and side effects certain contraceptives can have. As well as the side effects they experience along with illnesses and fertility issues, with lots of people not realising that these side effects are caused by the methods of contraception they’re taking, this can take a toll on both their mental and physical health. So, when looking into women’s health and how it is being impacted it’s obvious that not enough conversation is being had, including in personal relationships, with healthcare professionals and in education.
This article then is to explore contraception from many women’s own experiences, to highlight the issue that contraception needs improving, as does education surrounding it. It will also be analysing the study I’ve created based on contraceptive health and education and I shall explain its history and some of its complicated science.
I want to find out and raise awareness of how women’s health is being affected by contraception and how lack of education is such a huge factor. I will also be speaking to various individuals including members of the public and professionals.
I interviewed Doctor Aurore Malet-Karas, a neuroscientist and sexologist about contraceptives, it’s history, their effects on the body, and education, and she will be referred to throughout this article.
So, let’s begin with my truth. My experience with contraception has not been great, it’s been a long and winding road to try and find the right one for me, and ten years later, guess what? I still haven’t found the right one and I’m coming to the conclusion that sadly there just isn’t a right one for me (yet)!
It started when I was 15 years old suffering with awful painful acne and extremely painful periods, the GP wasn’t very informative or helpful and what I learnt in school does not prepare you for the different types of contraception out there, unless I want to put a condom on every banana. I was pretty much on my own with learning about this pill that was about to affect my entire body, so Google, books and scientific papers became my contraceptive best friends.
I didn’t experience the boob growth all my friends boasted about, but I did gain some weight, I felt like my mind was slightly numb, had mood swings and my acne didn’t clear up much either. I was thinking about stopping taking it but then my first boyfriend and I got more serious, so contraception became an obvious necessity.
So, I decided to try a different pill, to see if it improved and on one hand my acne did get better and my periods were lighter, although still painful, but on the other hand it wasn’t so good. I suffered from terrible mood swings, and at points depressed and suicidal, doubting myself and hating myself, which was very unusual for me. Even the alarm set for 7am every morning to take the pill used to infuriate me. Not only angry, but it also made me really paranoid which made me really unconfident and is not ideal when you’re 18 years old and your world is based around your looks, boys, socialising, job-seeking, and overall confidence.
It also ironically affected my sex life, I had no sex drive anymore, my vagina felt different to touch, it was dry all the time and sex became unpleasant, it gave me constant headaches which was another side effect of the pill I was unaware of. Then a year or so after taking the pill I decided it was time to give it up and not long after, the relationship I was in ended too (we will see later on how the pill can affect how you feel about your significant other).
Once starting uni and trusting only condoms I found myself in a situation where I needed emergency contraception. I was then recommended the copper coil (IUD) instead, not really knowing much about it, I jumped at the chance of a decade long hormone-free alternative. After an initial bumpy start of passing out on a London underground tube from the pain and a few days in bed with a hot water bottle and a lot of ibuprofen, the coil became my saviour. However, 18 months later I found out my IUD had moved and wasn’t as effective as it should be. On the recommendation of the gynaecologist, I had a replacement inserted, dosed on paracetamol, ibuprofen and accepting all the pain relief they would offer (unlike the first-time round) including a painful injection in my vagina. Yet, after three weeks I experienced some awful abdominal cramps and sex was painful. My GP referred me back to gynaecology where they told me it had moved again and they removed it for a second time, this time with me on gas and air. I swore, I cried, and I squeezed the life out of the nurse’s hand, vowing off IUD’s too.
After months off of contraception, I tried the mini pill in preparation for the injection and then the patch, but both affected my head just as the original pill had but worse. I was now angrier than I had ever been and was paranoid about what the contraception was doing to me. After planning it with my Gynaecologist, I got another coil inserted via ultrasound to check it was inserted in the right place and regular check-ups to make sure it hadn’t moved. I still have this coil today, but the pain and discomfort are still there, especially around my period, ovulation and after sex, unfortunately impacting my sex life. Like a lot of people, I don’t know whether to put up with it as a fact of life or sack it all off and put my trust in condoms and keep tracking my cycle using an app and taking my Body Basal Temperature (BBT).
Wait…what is contraception?
So on to the facts, if you do not know what contraception/ birth control /fertility control is, it’s a method of stopping conception (a woman getting pregnant) after heterosexual intercourse. Methods include hormonal contraception like taking a hormonal pill (which works by stopping ovulation), sterilisation (like a vasectomy), behavioural methods (such as a woman tracking their monthly cycles and the withdrawal method), and barrier methods (like condoms) which is the only method that prevents again Sexually Transmitted Diseases and Infections.
Hormonal contraception, which will be the main focus in this article, is currently only available for women, but over the last 60 years, there have been clinical trials and research into making a male equivalent (we’ll come back to this later). In 2009, the World Health Organisation created a list of medical criteria for all forms of contraception that people must meet before being put on a specific type, yet there is often debate about hormonal contraceptives causing troubling side effects.
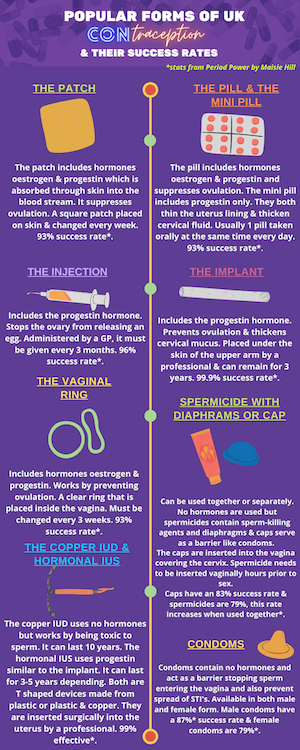
See the below graphic for a breakdown of the most popular methods of contraception in the UK and their success rates:
If hormonal contraceptives were newly invented and researched for women today, would they even make it through trials or be available?
Lauren Moult, 22, Stoke-on-Trent:
“From the age of 15 my skin and periods were bad, so I went on the mini pill. At first, I was prescribed Cerelle® which was fine apart from some mood swings. Then after a few months, they prescribed me with Cerazette®, which is a cheaper alternative, I noticed quite quickly all the side effects you hear about. I went back to the GP to swap back, but the nurse I saw was funny about it saying it’s literally the same, but I could tell it wasn’t. She prescribed me Desogestrel, but I ended up in hospital after having excruciating stomach cramps, throwing up, dizziness and a high temperature! They didn’t know what was wrong with me and put me on antibiotics which didn’t help. I went home and thought of what it could be, Googling the new pill I was on, it came up that other people had experienced it too! I stopped it immediately and three days later I was back to normal. I returned to my GP and told them what had happened saying I really needed Cerelle® which was agreed. Yet, when I went to get the prescription, they gave me Desogestrel, I was furious. It’s obvious the GP didn’t care what I’d been through. I gave up and ended up ordering Cerelle® online instead!”
Maisie Hill’s Period Power discusses the affect hormonal contraceptives can have on everyone, not just users. “With ingredients found in the pill found in our water supply, it is a concern for us all. The pill is an endocrine disruptor and because it is present in the urine of those that take it and water treatments don’t filter it out, we are all exposed to it”.
In particular hormonal methods such as pills, the implant, the hormonal IUS, the patch and injections, can all have both minor and severe side effects, but they can be beneficial too.
Let’s talk about the negatives first. Common side effects in these contraceptives can include migraines, stomach and abdominal cramping, lowered sexual desire, pain during sex, mood swings, acne, sore and swollen boobs, weight gain and bloating. As well as spotting, insomnia, higher blood pressure, irritability, blurred vision and problems with contact lenses, dizziness, leg swelling, increased vaginal discharge, nipple discharge, chest pain, nausea, increased hair growth, freckles and skin darkening, loss of head hair, depression, anxiety and vaginal discomfort.
Lydia Waller, 21, Hertfordshire:
“I came off the pill after experiencing bad mental health and weight gain, I was actually encouraged to do so by the GP whilst having a check-up for my blood pressure. Every time I went to see him, he told me that another woman at the age of 26 had died from having a stroke due to being on the pill. These are just not risks we’re ever really informed about, or not to these extremes. Long term as a young woman it can be really bad for you, it can kill you. I just really wanted some time just to know my own cycle, which I hadn’t known since I was 16.”
People on hormonal contraception also have lower levels of cortisol, which is having an effect on women’s stress responses, making them less able to cope with the stress. This is quite a new finding and there have been few studies into this, but it is currently being researched more to try and find out why this happens.
Maisie Hill discovered that some pill users will find that it also impacts on their ambition, motivation, and creativity and some will experience a destruction of them “and that has a huge consequence for every part of life”.
Claire Halligan, 21, Loughborough:
“I started on the pill when I was seventeen and soon had to come off because my mental health was really bad, I was always angry and crying. I decided to go on the copper coil (IUD) as I didn’t want any added hormones after the pill. The procedure was really painful and for a week afterwards, but obviously I thought it’s only once every 10 years. However, during my period a few weeks later I actually fainted a couple of times from the pain. I went back to the clinic and they couldn’t see it when they did an examination, telling me It had moved, and my body was doing mini contractions to have it pushed out. I then had to have it taken out which was extremely painful and so invasive, I cried so much. I’ve just been off all kinds of birth control and winging it at this point because I really don’t know what my best option is”.
A 2016 study of a million women on hormonal contraception in Denmark by Skovlund, Mørch, Kessing and Lidegaard, showed that 50 percent of women on hormonal contraceptives were diagnosed with depression and 40 percent being prescribed antidepressants. Shockingly women taking hormonal contraception were twice as likely to attempt suicide and three times as likely to successfully commit suicide compared to non-hormonal contraceptive takers. This is particularly true for young women between the ages of 15-19!
Some hormonal contraceptives such as the pill can also increase your risk of some cancers, including breast, cervical and liver, and it shouldn’t be taken if there is a history of breast cancer in your family or if you smoke (because of an increased risk of blood clots, which are more common in contraceptive users). Hormonal contraceptives also lower production of testosterone and DHEA. As well as decreasing bone density. They are linked to inflammatory bowel diseases such as Crohn’s disease and can lead to a heart attack or stroke.
However, it’s worth noting that with most medicines there are always side effects connected to them, from paracetamol to prescribed antibiotics, and the same with hormonal contraception, everybody can react differently to them. So when discussing hormones, it’s important to understand that because it’s a medicine they will never be free of side effects.
Harriet Davies, 21, Norwich
“I have taken the combined pill, the mini pill and had the implant, all of which caused me visual painful migraines, pins and needles in my hands and funny vision. Every time I went to the Doctor, they kept telling me that it was normal, and I just needed to wait it out, but it just wasn’t stopping, and I ended up really anaemic because of it!”
Because of the way different methods of hormonal contraceptives are administered they are unable to target just the genitalia or reproductive organs, meaning our entire bodies are affected because the entire body receives these hormones. Doctor Aurora discussed this with me through a simile; “how contraception works is like spam when you want to write a letter to someone you just write it to their address and I only want to write a letter to you. Whereas junk mail or chain emails are where they just send it and everyone gets it no matter who is interested, some will click the advertisement the ones who are interested but everyone still gets the mail regardless. It’s exactly the same when you are playing with hormones, the whole body receives the hormones and that’s why it’s a problem, it’s not only the genitalia touched by them but also parts of the brain, the heart, the lungs, it’s also the limbic system. So that’s why it’s really still a problem, especially as scientists still don’t know the full effect of what these hormones do to our bodies even after all this time. And that goes for the pills, the patch, the injection, the implant, all of them.”
Not only this but a study by Doctor Sarah E. Hill talks about how the brain is impacted on hormonal contraceptives; “up until recently little attention has been paid to what hormonal contraception is doing to the brain and therefore what it does to a woman as a person”. There’s been such a focus on safety (which is of course very important and should be considered), but it has not considered the rest of the body. There are areas of the brain that are responsible for things like “emotional processing, social interactions, attention, learning, memory, facial recognition, self-control, eating behaviours and language processing” and they’re all affected by hormonal contraception. As well as affecting other body parts like the immune system, the stress response and gut hormones, meaning the pill will have many different effects on your body as a whole. Is it starting to make a little more sense now?
Ellie Johns, 23, Dorset:
“Originally, I tried the combined pill, but I got headaches and because I’ve previously experienced blood clots I was never supposed to be on it. I then tried the progesterone only pill which made periods really heavy and painful, so I was advised to switch to the Mirena® IUD. The fitting was really uncomfortable and painful, I definitely didn’t feel like I was given enough preparation or information. On the day of insertion, I was told they wouldn’t fit it if I’d had sex in the previous seven days, but no one had told me that before and I had, but we proceeded anyway. I was bleeding really heavily for around four days and was bed ridden as it was so painful. I had had the IUD in for around three weeks when I started experiencing leg pains, I went to see my GP about it, where they weighed me, and I had gained a stone in weight since my last visit which was just before the IUD insertion! However, they wouldn’t confirm that it was from the coil despite me showing them my food diary and exercise routine which I should have been losing weight or at least staying at a steady weight. They encouraged me to keep the coil in for another four months despite the excruciating pain I was experiencing and continuing to put on weight. After six months I demanded they remove it and I felt better within a week, with no more pain or weight gain.
We’ve all heard that sex can be massively impacted by hormonal contraceptives too, but recent studies show they can affect your life by how you perceive your partner and your sex life. Choosing a partner when you’re on the pill appears to predict less long-term attraction and sexual satisfaction than what you might get from a relationship starting if you were not taking the pill. During my interview with her, Doctor Aurora even talks about how it can change women’s view of their partner and their smell. She says this is a concern for doctors; “the problem is that many medical doctors are not even aware of this impact because it’s not the same field in medical research as in practical research, so they cannot explain that to women and therefore change the pill or adapt the contraceptive for the woman.” In many cases, it can result in the end of a relationship, so it really is worth considering this and thinking about if you should take a break from contraception to discover if you’re still into your partner!
According to the study Relationship satisfaction and outcome in women who meet their partner when using oral contraception they found that sexual arousal, sexual adventurousness, sexual proceptivity, sexual attraction, partners support and partners body attractiveness were all ranked with higher satisfaction if you do not take the pill, and less satisfied if you do. However, orgasm’s with partners, partners loyalty, partners ambition, partners rejection, compliant sex and partners facial attractiveness were ranked as no different whether being on or off the pill. Research also shows that hormonal contraceptive users tend to have less sex and are more likely to have problems with pain or discomfort from sex than people who are not on hormonal contraceptives.
Alanya Wilson, 21, Cardiff:
“I was put on the pill at 17, and I bled for three months solid, when I went to see my GP about it, they said to persist for another three, but nothing changed. I then told my mum about it who took me to the doctor straight away as cervical cancer runs in my family. Having to come off the pill I got the injection where I bled solidly for nine months and the GP wouldn’t do anything. I decided to come off contraception for a while as it was taking a toll on my relationship and being intimate because of all the blood and feeling so unsexy. Then I booked in to get the copper IUD and it’s the best thing I ever did, the bleeding has stopped now, and I do have regular periods! However, I do bleed every time I have sex, I’ve been to the doctor’s several times about it, but they’ve told me there’s nothing that they can do. It’s sad that I have to accept that I will probably bleed every time I have sex until I want a child. Especially when in this society it’s taboo for boys to wear condoms or they are seen as gross, but I have to go through what I have just to make sure that I don’t get pregnant”.
Hormonal contraceptives can also cause a shrinking effect on our genitals and a fall in lubrication. It causes the labia minora to decrease in thickness, the size of the entrance to the vagina, less frequency of sex and lower occurrence of orgasm, as well as an increase in pain during sex. So, it’s really not great for our sex lives!
It’s also important to realise that progestin-only hormonal birth control contains just progestin (a synthetic form of the body’s naturally occurring hormone, progesterone) and the combined-hormonal birth control contains both progestin and a form of oestrogen, also synthetic hormones that replicate natural ones, meaning the body is now suppressing all of the natural hormones our bodies naturally create. In relation to periods and women’s menstrual cycles, Maisie Hill says “when you take these forms of hormonal contraception, you’re not taking oestrogen and/or progesterone, you’re actually taking a synthetic version of them. These aren’t the same and it also means you’re not getting all the benefits associated with the form of these hormones that you produce naturally as a result of your menstrual cycle”, it also means you’re not getting a real period. You may have a withdrawal bleed though, which happens, for example, by taking a break for a week once a month when on the pill. Many people think is their period, but you don’t naturally get a period if you are taking hormonal contraceptives, which many people are unaware of, including many of the women I spoke to for this project.
Hormonal contraceptives also aren’t great when it comes to fertility, when ready to ditch contraceptives altogether to start considering getting pregnant the lasting effects of the contraception can prevent that or at least take longer for it to happen. An association between long term hormonal contraceptive use (such as five to 10 years) and a thin uterine lining has been discovered which means it can have a negative impact on your ability to conceive. It often takes women a few cycles to get pregnant after they have stopped taking contraception especially if they have been on it for several years, so you should definitely consider tracking your cycle and coming off the pill for a few cycles before you’re ready to have children.
Shannon Wood, 22, Manchester:
“I first went on the combined contraceptive pill when I was 15 and it was initially to regulate my periods and pains. It caused really bad headaches, so I came off it for a while. When I went back on, I started to feel depressed and I was so explosive, silly things would make me angry and I couldn’t control my emotions. I wasn’t sure whether it was external factors or the pill itself. After a little while and after discussing it with my friends I found out it was because they had given me a cheaper version of the same pill, so I decided to go on the Hormonal IUD. I definitely think it has been the best choice for me, although my period pains and PMS are still quite bad.”
However, there are always two sides to every story, and we cannot forget that hormonal contraceptives do have positives for many women too. So on the upside, the pill has been shown to protect against cancers of the ovaries and the womb lining, as well as protecting against pelvic inflammatory disease which can be a painful infection which is hard to treat and can be a major trigger of women’s infertility (these are actually commonly caused by IUD and IUS insertion and removals).
Rebecca Cruz, 26, London:
“I went on the pill when I was 14 and have been on it ever since, occasionally having a break, it’s been a very positive experience for me, I haven’t had any of the side effects you usually hear about and it does the job.”
They are also prescribed for acne, painful periods and heavy bleeding (although they often cause this too). They are also known to help premenstrual syndrome (PMS), premenstrual dysphoric disorder (PMDD), polycystic ovaries (PCOS) and are helpful in treating endometriosis, which is why many people use them.
Amy Fenwick, 25, Hull:
“Hormonal contraception has massively affected my life and that’s why I decided to no longer use them and now use condoms instead because they don’t affect my body internally”
In many women, hormonal contraceptives have the reverse effect on their mental stability as previously mentioned, with some reporting that they feel more stabilised and focused when on the pill, giving them a clearer head and less emotional, especially around the time they would usually have their period.
Plus, we cannot forget, its main purpose, that means millions of women around the world are having liberated sex and are (mostly) not getting pregnant, revolutionising sex for everyone.
This leads me to the non-hormonal method of the IUD, also known as the copper coil. Not only a choice for non-hormonal contraception, but the copper IUD is also a method of emergency contraception (like the morning after pill), that can be used in an emergency for up to 5 days after unprotected sex and is 99.9 percent effective. Making it the most effective emergency birth control but also the most effective contraception too. It possesses many benefits including lasting for 10 years, meaning (unless needing to protect from STDs by using condoms) you do not need to worry about remembering contraception or having to order more. Plus, it does not have many of the side effects associated with hormonal contraceptives.
Abigail Eastep, 24, America to Liverpool:
“I have a hormonal IUD that I’ve had for about 3 years now, overall it’s been quite a positive experience. It was very painful to insert and for a month afterwards, but it lasts up to 5 years so it’s better than experiencing regular side effects such as the pill”.
But, because there is always a but, it can also have troubling side effects too. For example, Copper IUDs increase blood flow to up to 50 percent after insertion, for the first year and although periods then return to normal in many women, it isn’t the case for all, meaning heavier periods, and often more painful stomach cramps and heightened period symptoms. Bacterial vaginosis, pain after sex, and risk of pelvic inflammatory disease is higher too (although usually only if you have an infection such as chlamydia), this can be very painful and cause fertility issues. Not only this, but there is also a risk that the IUD can fall out. According to Lara Briden, author of The Period Repair Manual it’s commonly higher in the first couple of months after it inserted to move or fall, this then decreases to 2 percent per year. If not noticed it could result in pregnancy, but things to look out for include checking your strings, or any pain or spotting that seems unusual, you should get it checked with your gynaecologist if you believe it may have fallen or experience these.
Contraceptives through time…
An article by Malcom Potts and Martha Campbell provides a timeline of contraceptives through history. Starting from the ancient Egyptian times it was known that women would “insert fruits, pastes, jellies, acids into their vaginas to stop themselves getting pregnant, and from as far back as 1564 Gabriello Fullopious created a sheath to protect against STI’s, but a more recognisable condom style of contraception was created using animal intestines from the 18th century onwards”.
In 1882 Doctor C Hasse invented a type of diaphragm, followed a year later by Aletta Jacobs creating the first cap from the Netherlands, allowing Victorian women to control fertility for the first time, and then in the early 1900’s female condoms were created with rubber.
In 1909 the first specific IUD was created using silkworm, yet it is said that similar contraceptives were used by the ancient Greek’s. The 1960’s also saw the invention of the plastic IUD and later, the copper IUD.
The 60’s is often remembered for ‘The Pill’, which is the most popular form of contraception in the UK and was revolutionised in the 1960’s, the time of miniskirts and sexual liberation. 1961 was the year they were approved for use in the UK available from the NHS to married women, but each pill was equivalent to seven of today’s pill (imagine those side-effects)!
In 1967 it became available to all women. A year later the Pope Paul VI condemned the contraceptive pill in “an encyclical, Humanae Vitae” In a press conference at the Vatican (this is repeated in 2008 too).
In today’s society opinions on sex, relationships and religion have changed since the 1960’s and contraceptives are now more widely accepted. However, other ways contraception has changed from the 60’s to today is slightly slower than the progression of previous years leading to the 60’s. There have been thousands of clinical trials all over the world, researching various new methods, looking to improve some other methods and into their respective benefits and risks.
In 1984 emergency contraception, commonly known as ‘the morning after pill’ was made available, and in 2001 it was no longer required to have a prescription to get it, making it more accessible to many women.
When discussing history with Doctor Aurora she tells me the background of the hormonal contraceptives (mostly relating to the pill) and why it still falls on women, “It’s worse for women because we are of course in a patriarchal society and have been since the Roman Empire, so we are supposed to be at home and taking care of the children and it should be our business, the consequences are that we as women have to deal with it and the men don’t want to hear about it”. However, it was actually designed for men, but they took it and said the side effects were so bad that they refused, companies then changed the formula and tried giving it to women who then said the same. Yet, because so much money had been invested into the pill they needed to sell it, so it was sold to mental institutions where they actually they gave it to female patients where they were given a lot of pills a lot of drugs anyway, and this is how we come up with the 99.9 percent effectiveness from trialling it on these vulnerable women. But obviously these women were not sexually active because of their mental state and lack of visitors allowed anyway. The story behind the contraceptive pill is pretty horrible and shocking, and also the dosage of the pill at the time was around 10 times stronger than it is today, it’s crazy, they must have experienced such bad side effects I can’t even imagine”.
We can see from this brief history that practising safe sex and avoiding pregnancy has been thought about, talked about, researched and trialled for thousands of years…. So why are we still not quite getting it right for everybody?
“Education for both genders should promote the societal norm that, unless conception is planned, sex may be a feature of a good relationship only if adequate contraception exists.” – John Guillebaud
As of 2015, 81.3 percent of the UK used contraception compared to 69.2 percent of Europeans, according to Connor Stewart, “the main reasons for individuals attending sexual health services are to obtain information on available contraceptives, to ask for sexual health advice and to receive contraceptives”, showing there is a want from the UK public to learn more about contraceptives.
During the education section of my survey, it became clear the majority of participants do not believe they learnt enough in schools or higher education that allowed them to make an informed decision on contraception, which method may be right for them, or how it can impact on their health, relationships and ultimately their life. This is shown in my survey with a huge 51 percent saying they learnt a little but not enough in schools, with a shocking 41 percent saying they had not learnt anything at all!
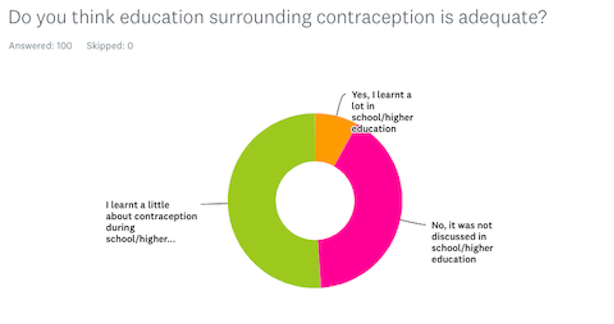
I then asked how they received any information surrounding contraception if not in school and 15 percent answered they have had to rely on their own research into forms of contraceptives, 23 percent have gained their knowledge from their GP’s, and 19 percent said they received all their contraceptive education through family or friends.
Amy Swiggs, 22, Exeter:
“The different options of contraception taught at school were very base level. I didn’t even know something as basic as the size of my uterus or female anatomy. I didn’t know what an IUD was, it sounded like a scary contraction, all I really got taught about was condoms”.
Finally in the survey, I asked: “if there was more education surrounding contraception from either GP’s or schools, do you think it would help women make more informed choices and potentially suit their health better?” 90 percent of participants answered yes, with some commenting that this should be “essential”!
As seen in the survey and testimonials above, when speaking to pretty much anybody I know they all say the same about their sex education, it was some embarrassing story of the biology of how girls and boys bodies work, what happens in puberty, how to put a banana on a condom, insert a tampon and the grim pictures of STI’s we must all avoid. Any conversation surrounding other methods of contraception are brief if there are any at all. But with casual sex and relationships less taboo than ever before, why are young people (yes, boys included) not taught about other forms, the importance of talking about it in a relationship? Especially considering the side effects many women experience and have trouble with, but also the benefits that contraception can provide for many people too.
Some say it’s all down to time, that many teachers do not have the time to teach this along with the rest of the UK curriculum, some say it’s an unwillingness from ‘older teachers’, some say it’s the parents not wanting their innocent little children learning about sex. Perhaps it is a combination of all of the above, but as you will learn from the testimonials throughout this article and the video below featuring a range of women, many would have spent more time researching/experimenting with different forms of contraception or even not taken any at all if they were made more aware of the risks, side effects and gained confidence and understanding out of the education system. I sure know I would have.
Rachel Bate, 25, Swindon:
“As a teacher, I do think there needs to be more education, I think most kids in years 10 and 11 know all the types of contraception but there’s not anywhere near enough education about how it affects the mental and physical health or the risks. I think some students are probably aware of weight gain but aren’t aware of the strong correlation between mood swings and longer-term or more serious side effects between women and hormonal contraceptives”.
The majority of women I interviewed said they also did not learn very much from GP’s either, some even saying they were practically pushed into taking the pill as a “tick box exercise” and told to read the leaflet. Some had better conversations with their doctors learning a little more and being told about cancers, blood clots and high blood pressure. Sexual health clinics and Gynaecologists are where many interviewees learnt a great deal about their contraception and side effects and benefits. Finally, the good old chat with friends and sometimes family were where the majority of women said they learnt the most about contraceptives and their effects, often not until later in life after leaving school.
Thankfully, as of September 2020 (COVID-19 pending), ‘Relationships education, relationships and sex education (RSE) and health education’, has been revised and will now be compulsory in UK schools. Seeing as many young people do not know about the different forms of contraception but 65 percent of children have seen hardcore pornography by the age of 15, it’s about time more sex education is needed.
When looking at the government’s guidelines on “what pupils should know ‘by the time they have left secondary school’” in relation to sexual health and relationships they do already cover; pregnancy, sexual exploitation and dangers, STI’s, how alcohol and drugs can affect sex, and even how all forms of health (mental, physical, reproductive) can be affected. In terms of contraception, “the facts about the full range of contraceptive choices, efficacy and options available” is now on the list to be taught, which is a big step in the education system.
Hollie Singh, 30, Swindon:
“Schools and GP’s need to be more aware that there’s a lot of underlying issue’s many people go through relating to contraception that people don’t realise. They don’t teach you in school that hormonal contraceptives are full of fake hormones that replace natural ones. Personally, I’m never going to go back on hormonal contraceptives, I don’t want to put them in my body. I never would have if I knew how damaging it was, I nearly couldn’t have children because of it. During school, I had one lesson about contraception, basically just on the different types and it was just the girls in the class which I think is horrendous, boys should know everything about women’s contraceptives, as we do for men which is just condoms, full stop. I also think it’s very taboo for a woman to go and buy condoms, I personally wouldn’t do it as it’s seen as embarrassing and that stigma needs to end.”
However, it is worth remembering that most schools have flexibility on what they decide to teach and when, as the above list is a guideline, so hopefully, it will be seen as an important matter to cover alongside other aspects of sexual education and not pushed to the wayside with busy school schedules like it was when it came to my sex education, learning more from famous Netflix show Sex Education than from school.
I also discussed education with Doctor Aurore, she tells me that in Europe and Western countries there is general sexual health education where every child should have free three hour sessions per year of sexual education, it’s the law in France, but it’s not applied because it’s left to the decision of the school director. “The programme on sexual education was made with UNESCO and big NGOs, it’s been sought globally so that every woman in western countries has the same background in education, including to learn about sex equality, domestic violence and communication too”.
Emily Greatrix, 22, Winchester:
“I think there’s a big lack of ceducation in schools as it really revolves around the biological aspect of sex and condoms at the maximum, which is just not broad enough, I think there needs to be a big improvement”
Doctor Aurora also adds, “what is going on now is very interesting, in that many people are taking the matter into their own hands, they’re writing books, making YouTube channels and there are now more and more resources about sexual education in general. We can see that more women are fed up with feeling disempowered with their bodies, so they are doing something about it themselves. I have also seen increasingly that men between 20 and 35 are more interested, involved and aware of the problem and of the side effects too. They seem concerned and interested, which wasn’t the case in previous generations, so I’m actually very positive about the future of contraception and where education and societal views are going”.
I agree with Doctor Aurora, this is a positive step forward and will help many women. Although, I still believe that it shouldn’t necessarily be the women’s responsibility at all times to have to research this. There should be proper education in place from the relevant age with more detailed and easy conversation with health experts so that each woman can properly find out about and explore the right option for herself, without being rushed or forced onto something that isn’t suited to them.
Heather Shore, 22, Nottingham:
“In school, I didn’t learn anything about contraception except that boys should wear condoms. In reality that isn’t always the case, more often than not boys are reluctant to wear one or even have one, and some people are allergic to latex. I’ve learnt everything myself through online forums and YouTube videos. Even when I see GP’s they aren’t very informative and usually brush off the mental health and weight gain effects. I think there needs to be more education on contraception in schools, with how GP’s approach the topic and also more development into non-hormonal and men’s contraception.”
Doctor Aurora and I then discussed her opinion of health practitioners’ knowledge surrounding contraception and the education they can give; “I would say that no medical doctors know enough right now, although it’s kind of changing for the young GP’s because they are aware of the issues and there have been a lot of scientific publications”. She also adds “I remember being 19 and visiting my gynaecologist, she said “you cannot get rid of the pill, it’s such a victory for women, you should be proud of it”, I’m not the only one who’s heard that from a gynaecologist either. For many women, it was such a breakthrough and freedom to really own the power of their bodies and sex lives that they did not actually really look too much into the side effects or maybe just didn’t want to look, but that needs to change”. It’s really difficult for the older generation of both gynaecologists and GP’s, she continues, but the problem is broader in that we have the same problem for any area of medicine because there’s a big gap between research and practical medicine. “Medical doctors don’t have time to look into the research and it’s really a general problem. This is what needs to change now, although things are changing for the better”. She believes that we need a solution for public policies for doctors, so they can adapt their practices for their clients and women concerning contraceptive health.
Sara Rafaty, 22, The Midlands:
“I think there needs to be more information given to people about contraception including males and especially from a young age. I definitely had no idea about what contraception did or how the hormones work and how they’d affect me. I went to a Catholic school, where we didn’t even get shown how to use condoms, so I do think there should be a more mandatory education implemented in the system for every type of school and higher education facility.”
It’s also been apparent during my research that we are not educated enough on the menstrual cycle and women’s anatomy, as well as contraceptives. Many people, including many of the women I interviewed for this project are misguided, uneducated, or factually incorrect, but I fully understand this is because we’ve never been taught the basics. I myself used to be included in this before I took it upon myself to really research and educate myself about this and to track my own cycle.
When discussing education, it’s also necessary to mention how contraception is often harder to access and talk about for Black, Asian and Ethnic minorities (BAME), as well within certain religious groups. There needs to be more effort by everybody to acknowledge and change this and more of an understanding that there are additional barriers some groups are facing when trying to access sexual health services and reproductive rights. Conversations need to be opened up in homes and relationships, as well as within health services.
The organisation Decolonising Contraception state in their Metro article, written by Neha Pathak, a member of the organisation, that only 8.7 percent of Black women versus 61.4 percent of white women pursue contraception from their GPs. South Asian women are also suffering from taboos when using sexual health and reproductive services, with 51 percent of South Asian women reporting they’re less likely to attend sexual health clinics if symptoms improve on their own. The reasons for these inequalities are not entirely clear but it’s most likely linked to history. Neha Pathak continues in the article that “colonised populations have had their reproductive freedom cut throughout history”. The shocking truth is that “Puerto Rican women were experimented on during clinical trials for the modern combined contraceptive pill, Black Americans have an extensive history of forced sterilisation and over six million Indian men were sterilised in 1976 alone” (2019).
It is also key to note from Maisie Hill, that the Depo-Provera® contraceptive injection is pushed on African American communities with 18 percent of black teens on it compared to only 9 percent of white teens. Plus, it’s currently used in sex offender rehabilitation centres to decrease the sex drive of offenders, and studies point to a link between using Depo-Provera® and an increased risk of HIV infections, which it is both important and worrying to be aware of as it is pushed in sub-Saharan Africa which has a high rate of high HIV transmission!
Women are only capable of conceiving six days in a cycle, so why are we the only ones bearing the load of drugs and devices?
This brings me on to male contraceptives! We’ve all heard that there have been clinical trials since forever, that men won’t be trusted or can’t deal with the side effects that women have to bear. But I wanted to find out more about what really is happening with them, or if anything even is happening (don’t worry, it’s looking likely!), as well as interviewing several men on why they would or wouldn’t be interested in male contraceptives.
I asked about male contraception in my survey. Interestingly when asked if a male contraceptive was available, a staggering 52 percent of women answered that they would trust their male partner and want them to take it, whereas 32 percent responded they would not and eight per cent of all participants answered they were unsure. Showing that women not trusting men enough to help take control of preventing pregnancy is an outdated myth. Also, the majority of males who responded said they would take a male contraceptive if it was available, with only one participant answering they would not, again showing the eagerness and interest that men have in relation to contraceptives.
Mitchell Singh, 31, Wiltshire:
“Personally, I wouldn’t get anything like a vasectomy (until I’m done with children), it’s just too invasive even if they were to become more reversible. I’d happily take a male version of a pill though. But I would still wear condoms if not in a committed relationship because of the risk of STDs”.
Whilst researching into male contraceptives and finding similar papers, conclusions and confusing jargon, I discovered the Male Contraceptive Initiative (MCI), an American organisation focusing on research and looking into the development of different forms surrounding male contraceptives. Their mission is to reimagine and “bring an empowered, inclusive, choice-maximised world of contraception to people globally”. They also promote education and product development surrounding male contraception.
Currently, they are researching different forms of male contraceptives and not just the commonly talked about “male pill”. These methods include spermatogenesis which targets the creation and development of sperm, sperm transport which interrupts the journey of sperm out of the body, sperm motility which slows them from reaching their destination, and fertilisation to prevent the interaction between sperm and egg.
Ashley Fisher, 27, Swindon:
“I would use male contraceptives if they were available, even if there were some side effects. The reason being is that I think woman go through a lot in regard to both birth and pregnancy prevention and have for far too long, they don’t have an easy time with not always being able to find the right fit and suffering from side effects. So, for a male to help out and take away the pressure and the stresses that come with it would be a great thing and a huge step forward”.
They have carried out many studies and in 2017 published what they believe to be the biggest survey regarding sexually active men from the ages of 18-44 In the U.S in the last 10 years. Their consumer research report states that “85 percent of American men want to prevent their partner from getting pregnant, with 60 percent of those men wanting to take responsibility for contraception as their key reason for wanting a new male method to be available”. 82 percent of men whose partners experienced an unplanned pregnancy in the past are now interested in new methods of male contraception, suggesting the toll of unplanned pregnancies can take on partners and relationships, and the high rate that this can happen. Their report also states that “men are twice as likely to prefer a non-hormonal method to the 38 percent that answered they would prefer a hormonal method.”
Luke Stone, 22, Bournemouth:
“I would take a male contraceptive but only depending on the side effects and what it does to your hormones, I know they aren’t great for a lot of women and I wouldn’t want to go through the same experiences or put my body through those side-effects”.
I had an interview with MCI’s Research Director Logan Nicker and Executive Director Heather Vahdat to find out more about male contraceptives, the work they are doing and education surrounding contraceptives as a whole.
When asking about hormonal contraceptives Logan said;
“There will always be a tie with some form of side effects even if it’s not in reality but in biology. The viewpoint of the public will always associate hormonal contraception with side effects. Furthermore, there are some characteristics of hormonal contraception that make it not an ideal solution so for that reason our organisation actually focuses on non-hormonal methods of contraception.” Find out more about these methods in the video below:
The organisation continue to tell me “what people want are just options out there, if a female partner wants to use contraception then great, those options are there for them, but if for some reason that doesn’t work or they don’t want to, the options become very limited very quickly and what should make sense is for couples to communicate about this and to be knowledgeable about their own reproductive desires and reproductive abilities. They should be able to effectively communicate and be fluent in reproduction together and make a decision that makes sense between the two of them for their lifestyle. It’s obvious the tools for this just aren’t there right now to really enable communication and make men feel like they are part of the conversation”. Logan adds “I think that gives them an easy out a lot of times, some men just don’t really want to be a part of it and to be honest they currently have an easy way out to get out of it.”
When I asked MCI about education surrounding sex and contraceptives, Logan answered; “as a man, I think that men are especially ill-equipped when it comes to sex education, I know that a majority of men don’t know what IUD stands for. Where I grew up was a very conservative state and I got little education about what contraception was, and much less how to prevent pregnancies or how to just be literate in anatomy and reproduction in general”.
He continues to say that he thinks a lot of information is left up for people to figure out themselves and sex education is approached with this kind of ‘we don’t want to’ sort of mentality. It’s not nearly as open and honest as it should be, and he feels society in western cultures aren’t treating young adults like young adults by being too delicate, “we need to let them know that sex and contraception are a part of life and they are most definitely going to come up!” he adds.
“There’s this joke in male contraception that it’s been 10 years away for 50 years and it grabbed me because I’ve always wondered well why haven’t we been able to do this?”
Logan tells me the more he learned about the field the more it became a solvable problem to him, “it’s something that scientifically is certainly achievable and the barriers that exist for it are financial, technical and social, things that are complicated and play into one another, but they’re all things that can be overcome by people with time, motivation, and effort, and none of that had been there in this field before.”
His way of thinking about contraception relates to economic and societal benefits, saying that it can advance gender equity and society in all sorts of ways. Logan explains that male contraceptives have an unfair advantage because there isn’t one yet, and “just one male contraceptive alone is going to have a really large impact on society when it becomes available.”
On a personal note for both himself and other men he has spoken to, he explains to me that “contraception is something I’ve always felt on the side-lines within relationships, it feels almost emasculating to not be able to step up and be a part of this and unable to contribute to a partnership in something that’s a really key piece of a long-term relationship”.
In relation to the various opinions circulating around male contraceptives, I spoke to Heather regarding responses she receives when discussing male contraceptives with others, including random people, people she’s interviewed for studies or family and friends. She told me;
“With men that aren’t generally interested, it’s usually because they are worried and concerned with side effects, or there’s some masculinity part that they like to think that they are able to conceive at any given moment, like as a part of their masculine nature. But that’s such a minority response, I think the vast majority of men we talk to are interested and then there’s a lot of survey data to show that in any case about half of men say “contraception? Yeah sure!”.
She acknowledges that there, of course, will be people who won’t want to use it, but thinks they will be the minority, “and that’s fine we want everybody to use what works for them, that’s the point” she says.
I then asked the golden question; how long will it be until a male contraceptive is on the market and what will it be? They tell me it is a complicated answer, one they are often asked. Logan says “as it sits now a drug-based male contraceptive is likely around a decade away (I know this is always what everybody says), and that’s for the ones that are being tested in clinical trials right now. Other methods, like those that are in preclinical studies, are likely further away. That timeline, while measured in years, is likely shorter than the decade-plus for drug-based methods. However, medical devices, like the vas-occlusive methods mentioned in our video, could be closer as their regulatory pathway is quite different. We’re quite excited about these methods as they have the potential to provide years of “set-it-and-forget-it” protection”!
Alex Grahame, 27, London,
“I’d be interested in a male contraceptive and I don’t think it should be a women’s responsibility. I would personally see it more as liberating than a reliance on somebody else. I went to an all-boys school so anything regarding contraception or sex education was seen as hysterical, I don’t know how much content was really absorbed at those times, I do remember there being quite a decent effort from teachers though, which I’ve heard is unusual in this country. But, as a man you have to teach yourself, I’ve learnt a lot since school, absorbing information from partners. I don’t think it’s good enough to say, “oh I know about it” and then just never research it or come to speak about again. It’s something we as men should speak up about more, and as a society it should be an ongoing conversation”.
If you’d like to find out more about male contraception, the background and the history, listen to MCI’s captivating podcast: INTENDED.
So, is contraception a Con? (pun intended!)
I already knew that opening up a conversation surrounding contraceptives, the lack of education surrounding them and the impact they have on women’s health was a vital conversation that needed its lid flipping open, but research and testimonials from this article have proved that to progress and improve contraceptives an in-depth conversation must be had!
Contraception has been around for thousands of years, it has been trialled and tested, written about, and has been a day to day burden for women since the 60’s, we know this, and we also know it isn’t working right for many women. Yes, there are of course benefits and it has allowed us a sexual revolution with a way to enjoy sex without the worry of conceiving. But, and it’s a big but, women are experiencing horrific symptoms, illness and even death that can be linked to contraceptives – either from suicide rates increasing or relating to heightened blood clot and risk of stroke. Something needs to be done and education needs to be at the forefront of conversation, especially between healthcare professionals and us women. Our male partners to need to understand what we are going through, the different options to try, and the health risks and benefits. This is NOT just a women’s issue, it’s a general health issue and the sex taboos that come with it need to be dismantled!
It has become both clear and vital to me through this article with its statistics and testimonials that more needs to be done and I hope it is now clear to you too.
“When women go on hormonal contraception which changes who they are and what they do, it can influence other people by changing who they are and what they do too. Therefore, the pill (by changing women) has the ability to have a cascading butterfly effect on everything and everyone a woman encounters, and when you multiply this type of effect by several million (the number of women around the world on the pill), the pill changes the world!” – Doctor Sarah E. Hill
I asked Doctor Aurore if she had any last bits of advice for women reading this and she told me something that should be really underlined for women is the importance of getting to know our bodies, the earlier the better, to get in sync with our cycle, learn about it and how we feel, track our cycles either on pen or paper or using an app. “Also, get off hormonal contraception and try to experience a few cycles without any hormones, just look at what happens, what happens before the period, what it’s like when you ovulate. This is something that every woman should do at some point in their lives just to get to know themselves better”. I too can vouch for this having done it for the last few years, it can really help your day to day life and also of course help if you’re wanting to get pregnant soon.
So I urge you to track your cycle if you haven’t already, consider your contraception options and do your research, because if something doesn’t feel quite right then it probably isn’t. Please persist with talking to your GP’s, chemists and if available to you a gynaecologist. If you don’t find the right one or think them unhelpful then request to see somebody else and don’t give up. Doctor Sarah E Hill says in her book to ask yourself questions when asking about starting new contraception too, such as:
- Do I feel like myself on this contraception?
- Has my behaviour changed since going on this contraception?
- How frequently has my mood changed?
- Has my relationship (both sexual and non-sexual) changed?
- Have my motivations changed since using it?
- Am I tired more often?
- Am I experiencing any pain?
- (And the big one) how do I feel about all of this?
I have one more thing to add… since beginning this project (and as mentioned earlier), I was questioning whether to keep in my cooper IUD, two days before this was sent to be published I went to get it checked out with a gynaecologist. I thought it had moved like my previous two and that’s what was causing me pain, it turns out I have been diagnosed with endometriosis, and my coil is perfectly fine. The irony of this? The only way to treat endometriosis is with hormonal contraception! This perhaps proves how complicated contraception and women’s health is. I’m now unsure of what my contraceptive future holds, but as highlighted in this article, having the best education possible will be sure to help me.
Contraception shouldn’t be a burden or a health risk, and the future of contraception and sexual health is exciting, and we should embrace that. Who knows, our male partners may be the ones on contraception sooner than we all first thought, freeing us temporarily once and for all (maybe)!*
*A last little side note to say, I was so surprised by the huge amount of people who got into contact with me, having to close my survey early, and with my hard drive full of people’s experiences and views, messages pinging at me all throughout the day. I am both shocked, saddened and cringing at some of the story’s women have shared with me and honoured they have done so. This has prompted me to continue this project to a frequent blog where I can share experiences, conduct interviews and podcasts, and continue to share my findings, your stories and experiences to continue the conversation surrounding contraception for as long as I can! So, watch this space… Project CON·TRACEPTION? is underway!
RESOURCES
PODCASTS:
INTENDED by MCI
https://open.spotify.com/show/0gB0mR4rMyb6u92k8pKaC8?si=ZDxW83CxTAODeJWXSuRCLg
The Sex Agenda Podcast by Decolonising Contraception
https://open.spotify.com/show/1L04Gg3IKMigOLNHOU6ZVU?si=w5wuf7vSTc219VRTMUzDcw
Hormonal by CLUE
https://open.spotify.com/show/5fBxybHNAi5lswBRyHU06d?si=WwsRyq18QI6j3YxG9O4kQA
#MYCONTRACEPTION by Bayer
https://open.spotify.com/show/44NfybBLBb7rNdi836Dcyx?si=yms3hED7RQyx_U3QnU4jJw
BMJ’s Sexual & Reproductive Health Podcast
https://open.spotify.com/show/2y28EfQz9vnXoTPTaCYHvb?si=4MX1z3pcSLuxYS60PtCeSw
All about birth control & your V, with Dr Sophia Yen
https://open.spotify.com/show/4jrzlieEImErRXxrvdtpSB?si=MQ0FX2oyTLqcR6NMpBsV0w
Contraception, and Contraception during COVID by RCGP:
https://podcasts.apple.com/gb/podcast/contraception/id1474942018?i=1000445768108
https://podcasts.apple.com/gb/podcast/contraception-and-covid-19/id1474942018?i=1000476784685
BOOKS:
How the Pill Changes Everything: Your Brain On Birth Control by Doctor Sarah E. Hill
Period Power by Maisie Hill
Sweetening the Pill: Or How We Got Hooked on Hormonal Birth Control by Holly Grigg-Spall
Beyond the Pill: A 30-Day Program to Balance Your Hormones, Reclaim Your Body, and Reverse the Dangerous Side Effects of the Birth Control Pill by Jolene Brighten
Woman Code: Perfect Your Cycle, Amplify Your Fertility, Supercharge Your Sex Drive, and Become a Power Source by Alisa Vitti.
WEBSITES:
https://www.nhs.uk/live-well/sexual-health/getting-contraception/
https://www.maisiehill.com/blog
https://www.nhs.uk/conditions/contraception/
https://flo.health/menstrual-cycle/sex/birth-control
https://helloclue.com/articles/birth-control
https://www.sexwise.org.uk/contraception
SOCIAL MEDIA:
@mycontraception
@decolonsingcontraception
@sxwise
@TheSexDoctorUK
@FSRH_UK
TOOLS:
https://www.maisiehill.com/chartmycycle
https://helloclue.com/
https://flo.health/